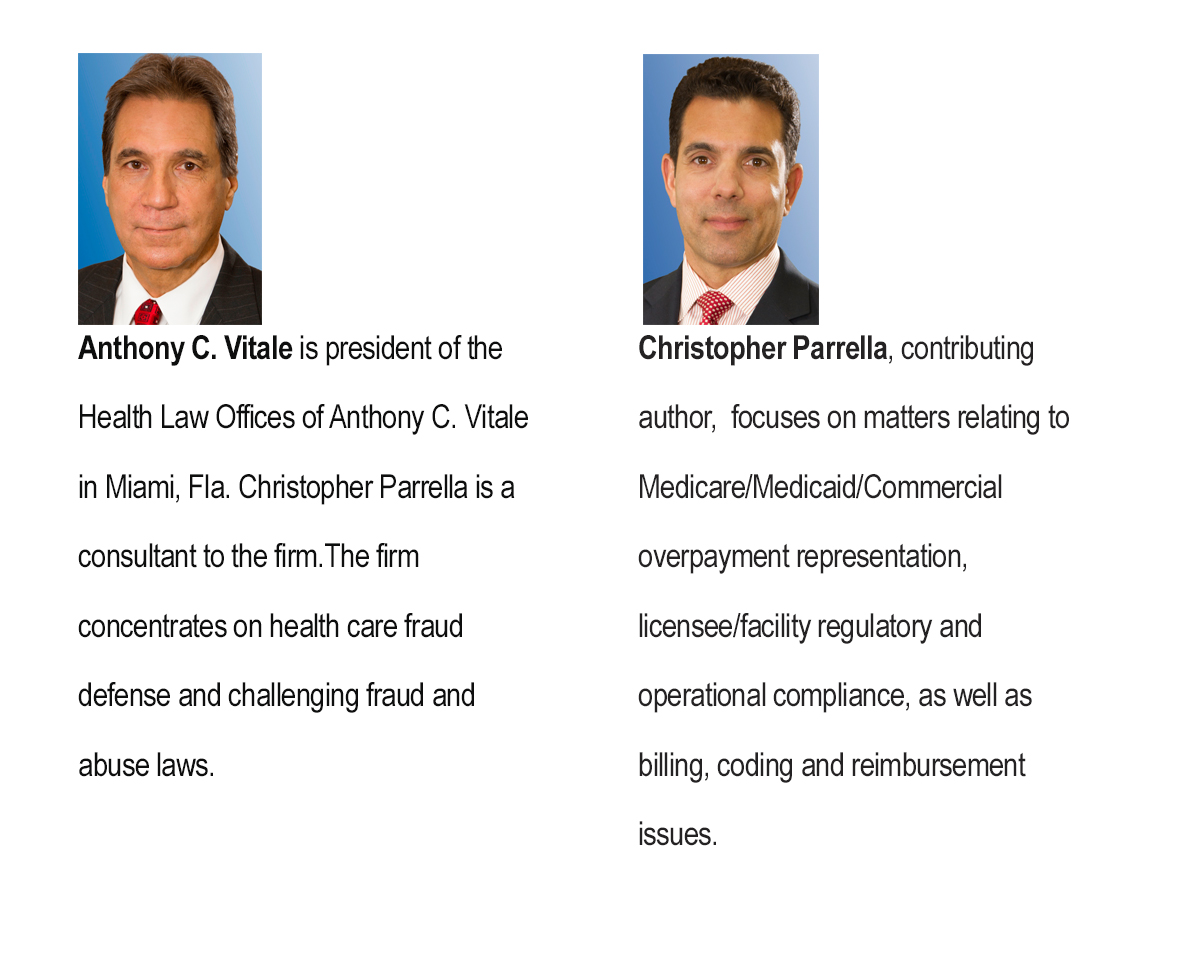
with contributing author Christopher Parrella
In mid-May, law enforcement authorities announced the arrest of 90 people, including 16 physicians, who allegedly took part in Medicare fraud schemes across the country at an estimated cost to taxpayers of $260 million.
David O’Neil, acting assistant attorney general, said the alleged crimes “represent the face of health care fraud today.”
Billing for services never rendered, providing medical equipment that was not needed and paying kickbacks to recruiters to obtain Medicare billing numbers from unsuspecting patients are just some of the ways these schemes are alleged to have taken place.
Although relatively big, the most recent crackdown is just a drop in the bucket when it comes to the government’s efforts to catch those involved in health care fraud. In fact, since 2007 there have been more than 1,700 people charged with Medicare fraud, collectively billing more than $5.5 billion.
Whether you are a solo practitioner or working within a large health care system, no one is immune from becoming the target of an investigation. That’s why having a compliance program in place, and a compliance officer to ensure that all regulations are followed, is imperative.
Because health care law is a field that’s constantly changing, it’s often not easy to keep abreast of all of the rules and regulations. This is even truer today with the implementation of the Affordable Care Act, better known as “Obamacare.” The Act has added tough new rules and sentencing for those convicted of health care fraud and calls for enhanced screening of providers.
As a result, there are several things you can do to make sure you remain in compliance:
- Hire an experienced health care fraud defense firm to review your business practice.
- Create a compliance program that describes how the practice will submit claims and handle administrative functions.
- Perform internal risk assessments relating to new enforcement areas.
- Audit internal records regularly to make sure that services are being properly billed and coded.
- Establish an anonymous employee hotline to report suspicious activity.
- Carefully review employee non-compliance complaints.
- Educate employees about procedures for preventing fraud and abuse and about new enforcement trends.
- Make sure your medical records are current as to the necessary information including procedure codes, place of service and type of service.
Health care providers must have a clear understanding of what is expected by Medicare, Medicaid and commercial insurers. It’s also imperative to be knowledgeable about their billing, coding and documentation rules and regulations, which can be found in the provider’s contract, handbook or by speaking directly with the payor.
There are several major federal fraud statutes and regulations designed to prevent health care fraud. They include:
The False Claims Act, which simply stated, prohibits the submission of knowingly false claims to collect federal money. Under this act, health care professionals and others can be liable for treble damages – plus civil penalties.
It’s important to note that under the qui tam provision of this act, private citizens can act as whistleblowers. If the government is successful in collecting money as a result of a whistleblower case, then the whistleblower is entitled to a share of the money.
The Anti-Kickback Statute is a criminal statute that prohibits the exchange, or the offer to exchange, anything of value in an effort to induce or reward the referral of federal health care program business.
The Physician Self-Referral Law is commonly known as the “Stark Law.” Essentially, it prohibits a physician from making referrals for certain designated services payable by Medicare to an entity with which the provider or an immediate family member has a financial interest unless an exception applies.
Exclusion Authorities refers to the fact that the Office of the Inspector General has the authority to exclude individuals and entities from federally funded health care programs and keeps a list of those who are excluded. There are many reasons for exclusions, including past convictions of fraud, financial misconduct, patient abuse or neglect and a number of felony convictions and other bases for exclusion from the OIG which are permissive in nature.
Civil Monetary Penalties authorizes the imposition of substantial civil monetary penalties against an entity or individual that makes a false claim, provides false or misleading information that is expected to influence a decision to discharge a patient, offers remuneration to a beneficiary of a federal health care program that is likely to influence the receipt of reimbursable items or services, arranges for reimbursable services with an entity that is excluded from taking part in a federal health care program; solicits or receives remuneration for a referral of a federal health care program beneficiary or uses a payment intended for a federal health care program beneficiary for another use.
Ignorance is not a defense in the health care fraud environment. Even an honest mistake can cost you time, money and your reputation. If you become the target of an investigation, the first thing you should do is contact experienced and competent health care legal counsel. They can advise how to properly proceed.